Safe antibiotics for use in pregnancy
Penicillin is known by several different names and is known to be safe. Common penicillin drugs include amoxycillin, cloxacillin and methicillin. There are many other types of penicillin. It is safe to use at any stage of pregnancy.
Another group of antibiotics which are not known to cause any harm to the fetus are the cephalosporins. These too are known in a variety of names. Those commonly used include cephradine, cefuroxime, cefotaxime, cefalexin, cefaclor, and cefadroxil.
Tetracycline in pregnancy
There are various types of tetracycline. These are known to be harmful in the second half of pregnancy, where they can be incorporated in the developing bones and the forming teeth. With the latter, the discoloration caused is permanent.
Even though the confirmed harm appears to be confined to the second half of pregnancy, the standard advice is to avoid them throughout pregnancy. This advice also applies to the period after delivery, if the mother is breast-
Trimethoprim in pregnancy
This drug, which is commonly prescribed for urinary tract infection, is frowned upon by most doctors when it comes to use in pregnancy. There is a theoretical risk, yet to be confirmed, that the baby may be harmed. This is based on the fact that it is a folic acid antagonist. Most doctors would prefer to use alternatives.
Trimethoprim is marketed under various names including Proloprim, Triprim, Trimpex, Primsol etc.
Septrin (Co-
Septrin is one of the well-
Gentamicin (and other aminoglycosides) in Pregnancy
Gentamicin is a powerful antibiotic belonging to a group of antibiotics called aminoglycosides.There is no known harmful effect to the baby if these drugs are administered during pregnancy. The consensus is that, since these have been in use for decades with no reported teratogenic or other adverse effects to the fetus, these are very unlikely to occur and, if required, these should be used.
Other aminoglycosides where similar advice applies include streptomycin, Tobramycin, Kanamycin and a few others.
Ciprofloxacin use in pregnancy
This is another powerful antibiotic effective against a wide-
Vancomycin safety in Pregnancy
Vancomycin is one of the so-
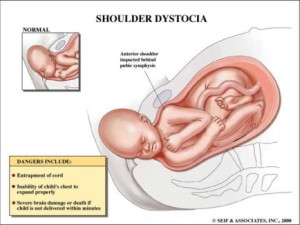 Shoulder dystocia is diagnosed when the shoulders get stuck at the pelvic brim when the head has been delivered.
Shoulder dystocia is diagnosed when the shoulders get stuck at the pelvic brim when the head has been delivered.